
By Mary Jane Minkin, MD, FACOG, NCMP
Clinical Professor, Department of Obstetrics, Gynecology and Reproductive Sciences, Yale Medical School
An educational grant to help fund this article was provided by Duchesnay USA.
Due to improvements in public health and medicine over the past 150 years, the life expectancy for women in the United States has increased into the late 70s, while the age of onset of menopause has remained at around age 52. This means that American women now spend approximately one third of their lives in post-menopause!
Healthy women transition from their reproductive years to menopause when hormone production in their ovaries drops to a level that is no longer sufficient to maintain ovulation and menstruation. 1While many women are happy not to have to worry about monthly periods anymore, lower estrogen levels can cause a number of other, less pleasant symptoms, including hot flashes, night sweats, bone loss, weight gain, mood swings and sleep disturbances. While most women are prepared for these symptoms, one symptom that often comes as a surprise is pain during sexual intercourse. Also known as dyspareunia, painful intercourse is most often a symptom of Vulvovaginal Atrophy (VVA) due to menopause.
What is VVA?
VVA is a condition in which low estrogen levels due to menopause cause a number of bothersome urinary and vulvovaginal (affecting the vulva and/or the vagina) symptoms. Urinary symptoms can include increased frequency, nocturia (waking at night to urinate), urgency, incontinence, dysuria (painful or difficult urination) and recurrent urinary tract infections.
Vulvovaginal symptoms can include irritation, itching, burning, dryness, light bleeding after intercourse, abnormal discharge and dyspareunia (painful intercourse).2
What VVA looks like
Physiological changes in the vagina due to menopause:3
- Increased pH level4
- Fewer superficial cells5
- More parabasal cells5
- Diminished blood flow to the vagina, leading to decreased lubrication5
Before menopause, the inner lining of the vagina is moist and thick with ridges (called rugae).
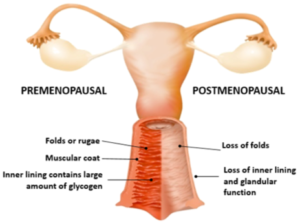
As estrogen levels fall during menopause:
- The inner lining gets thinner and loses its ridges.
- Increased parabasal cells and decreased surface (superficial) cells, making the lining sensitive and dry.
- Vaginal pH levels rise, allowing an overgrowth of harmful bacteria, which can cause vaginal infections and inflammation.
- Vaginal elasticity decrease and connective tissue increases.
- Lower estrogen levels decrease blood flow and lubrication.6
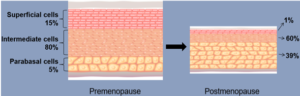
After menopause, a low number of surface cells result in the vaginal mucous membrane becoming sensitive and dry.7
With less stretchiness and less moisture, it is no wonder so many menopausal women find sex painful!
Impact of VVA Symptoms: the VIVA Survey
In order to determine what impact the effects of VVA were having on women’s lives, an international survey was conducted among 3,520 postmenopausal women aged 55 to 65 years. The study revealed that 45% of women (51% in the U.S.) reported symptoms of VVA.8
- 75% said that VVA symptoms had a negative impact on their lives
- 62% described their symptoms as moderate or severe
- Over half (55%) reported symptoms lasting 3 years or longer
 Why dyspareunia often goes untreated
Why dyspareunia often goes untreated
Despite painful sex being one of the most common symptoms of menopause, it is also one of the most under-treated. Sadly, many women do not seek help for this condition for a variety of reasons. For some women, it is a sensitive topic that they are too shy or embarrassed to discuss with their doctor. Other women think painful sex is simply an inevitable symptom of aging.9 Still others are under the mistaken impression that their symptoms will eventually go away on their own.8
Why treating dyspareunia is important
While some menopause symptoms, such as hot flashes, night sweats and fatigue, improve on their own over time, painful sex is a chronic condition. That means that without treatment, symptoms will not go away and may even get worse.10
As mentioned, women spend an average of 30 years in menopause. That’s a long time to suffer from painful sex! Fortunately, there is no reason to suffer, because a variety of treatment options exist.
Over-the-counter remedies
If you are experiencing painful sex due to menopause, you can start with an over-the-counter vaginal moisturizer or lubricant. Lubricants are short acting and used primarily at the time of intercourse. Moisturizers are longer acting and inserted vaginally two or three times a week. While these options are available at your local pharmacy without a prescription, they may provide temporary relief, but do nothing to treat the underlying condition that is causing your pain.
Using a vibrator may also help moisturize vaginal tissues by increasing pelvic blood flow.
When over-the-counter options are not enough
If over-the-counter remedies are not enough and you are looking for a solution that actually helps improve the condition of the tissues that are causing your pain, you have several options:
Vaginal suppositories
Inserted nightly, these steroid hormones are absorbed by the cells in your vagina and converted into testosterone and estrogen. The estrogen helps increase vaginal moisture, while the effects of the testosterone are uncertain, but it may decrease pain and/or increase libido.
Estrogen therapy
Estrogen therapy has been shown to be very effective at reducing menopause symptoms, including vaginal dryness and overall sexual functioning.11 Estrogen comes in many forms, including vaginal rings, vaginal suppositories (tablets), creams and gels. When used as directed, all three forms ensure that only a minimal amount of estrogen is absorbed by your body.
SERMs
SERMs are non-hormonal, synthetic molecules that work by binding to estrogen receptors in the body and have “tissue selective effects”.12 This means that SERMs have different effects depending on which tissues they are working in. In some areas of the body, SERMs bind to the estrogen receptor and mimic the effects of estrogen, without being estrogen. In other areas, SERMs bind to estrogen receptors and block the effects of estrogen. SERMs are used to treat a variety of medical conditions, but the one used to treat moderate to severe painful sex due to menopause is called “ospemifene”.
Sold under the brand name Osphena®, ospemifene helps counteract the changes in your vaginal tissues that resulted from low estrogen levels. By improving the condition of your vaginal tissues, ospemifene makes sex less painful. In other words, Osphena® provides the relief you need without hormones.
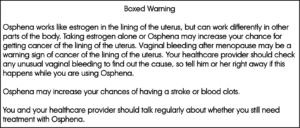
Osphena® may increase the risk of cancer of the lining of the uterus, so tell your healthcare provider right away if you have any unusual vaginal bleeding while taking Osphena®. It may also increase the risk of stroke and blood clots. You and your healthcare provider should talk regularly about whether you still need treatment with Osphena®.
In addition to being non-hormonal, Osphena® is the only treatment for moderate to severe dyspareunia due to menopause that comes in an oral pill. Many of my patients prefer taking a daily pill by mouth, either because they are uncomfortable using vaginal products that require an applicator, or because they are bothered by the staining and/or physical discomfort caused by vaginal treatments, which may also interfere with sexual spontaneity. Of course, this is a matter of personal preference, but only your doctor can determine if a specific treatment is right for you.
Start the conversation with your doctor!
 While menopause comes with many changes, a loss of sexual intimacy does not have to be one of them. I believe that sexual satisfaction is important at any age. Painful sex due to menopause may be a sensitive subject, but it is a women’s health issue that is simply too important to ignore. That’s why I regularly ask my menopausal patients if they are experiencing pain during or after intercourse. However, like every patient, every doctor is different, so if your doctor doesn’t ask, start the conversation!
While menopause comes with many changes, a loss of sexual intimacy does not have to be one of them. I believe that sexual satisfaction is important at any age. Painful sex due to menopause may be a sensitive subject, but it is a women’s health issue that is simply too important to ignore. That’s why I regularly ask my menopausal patients if they are experiencing pain during or after intercourse. However, like every patient, every doctor is different, so if your doctor doesn’t ask, start the conversation!
Indication and Important Safety Information
Indication: Osphena® is a prescription oral pill that treats moderate to severe painful intercourse, a symptom of changes in and around your vagina, due to menopause.
Most Important Information you should know about Osphena®
Osphena® works like estrogen in the lining of the uterus, but can work differently in other parts of the body. Taking estrogen alone or Osphena® may increase your chance for getting cancer of the lining of the uterus. Vaginal bleeding after menopause may be a warning sign of cancer of the lining of the uterus. Your healthcare provider should check any unusual vaginal bleeding to find out the cause, so tell him or her right away if this happens while you are using Osphena®.
Osphena® may increase your chances of having a stroke or blood clots.
You and your healthcare provider should talk regularly about whether you still need treatment with Osphena®.
Call your healthcare provider right away if you have changes in vision or speech, sudden new severe headaches, and severe pains in your chest or legs with or without shortness of breath, weakness and fatigue. Osphena® should not be used if you have unusual vaginal bleeding, have or have had certain types of cancers (including cancer of the breast or uterus), have or have had blood clots, have had a stroke or heart attack, have severe liver problems, are allergic to Osphena® or any of its ingredients, or think you may be pregnant. Tell your healthcare provider if you are going to have surgery or will be on bed rest.
Possible side effects of Osphena®
Serious but less common side effects can include stroke, blood clots and cancer of the lining of the uterus.
Common side effects may include hot flashes, vaginal discharge, muscle spasms and increased sweating.
Tell your healthcare provider about all of the medicines and supplements you take, as some medicines may affect how Osphena® works. Osphena® may also affect how other medicines work.
Duchesnay USA encourages you to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please read Patient Information for Osphena®(ospemifene) tablets, including Boxed Warning, in the U.S. Full Prescribing Information, at www.osphena.com.
Important Safety Information, including Boxed Warning, and Indication
Indication: What is Osphena® (ospemifene)?
Osphena is a prescription oral pill that treats moderate to severe painful intercourse, a symptom of changes in and around your vagina, due to menopause.
Most Important Information you should know about Osphena®
Call your healthcare provider right away if you have changes in vision or speech, sudden new severe headaches, and severe pains in your chest or legs with or without shortness of breath, weakness and fatigue. Osphena should not be used if you have unusual vaginal bleeding, have or have had certain types of cancers (including cancer of the breast or uterus), have or have had blood clots, have had a stroke or heart attack, have severe liver problems, are allergic to Osphena or any of its ingredients, or think you may be pregnant. Tell your healthcare provider if you are going to have surgery or will be on bed rest.
Possible side effects of Osphena
Serious but less common side effects can include stroke, blood clots and cancer of the lining of the uterus.
Common side effects may include hot flashes, vaginal discharge, muscle spasms and increased sweating.
Tell your healthcare provider about all of the medicines and supplements you take, as some medicines may affect how Osphena works. Osphena may also affect how other medicines work.
![]()

