Although ovarian cancer is uncommon, it scares us more than many other cancers because it usually doesn’t show discernible symptoms until it’s in an advanced stage, when there may be little to no hope for cure. Even though other cancers also don’t exhibit warning signs until their later stages—colon cancer, for example—screening tests can catch and treat them earlier and more successfully. Unfortunately, there’s no good screening test for ovarian cancer.


Since worrying or trolling the Internet every time we have stomach bloating or abdominal discomfort aren’t very effective, we asked Dr. Michael Randell, highly regarded Atlanta-based OBGYN at Northside Hospital, exactly what we need to know and do when it comes to this dreaded disease. His advice also is crucial for any of us who have sisters, daughters or nieces in our lives.
What is the incidence of ovarian cancer?
It’s estimated that 21,980 new ovarian cancer cases will be diagnosed this year in women of all ages and 14,270 women will die of the disease in 2014 (the latter figure represents women whose cancer was diagnosed earlier than 2014 since very few deaths occur the first year after diagnosis.)
- Stage 1: 24 percent of all ovarian cancers are diagnosed at this stage; these women have a 95 percent 5-year survival rate
- Stage 2: 6 percent are diagnosed with a 65 percent 5-year survival rate
- Stage 3: 55 percent are diagnosed with a 15 to 30 percent 5-year survival rate
- Stage 4: 15 percent are diagnosed with a 0 to 20 percent 5-year survival rate
Why don’t most women know they have ovarian cancer until it’s too late?
The symptoms are vague and non-specific, so patients are improperly diagnosed or not diagnosed and it’s dismissed. Even in more advanced stages, when a woman might feel bloating and abdominal discomfort with distention, have weight gain yet feel full after eating only a few bites, it can go undiagnosed if a doctor doesn’t do an adequate evaluation or workup.
If I experience these symptoms and they don’t disappear after a few weeks, shouldn’t I seek an aggressive evaluation?
Yes, you should. You need and want to find out what’s causing them.
And what kind of doctor should I see?
A great deal of health care today is being provided by mid-level people, who are not doctors–nurse practitioners, for example—and therefore women aren’t being evaluated by the proper physicians and too many short cuts are being taken. If you have symptoms that concern you, over a few weeks, make an appointment with an OBGYN who is trained and experienced in performing pelvic examinations. Actress Gilda Radner had these symptoms, but she didn’t initially see the  right doctors and didn’t have the right tests performed. Her diagnosis of ovarian cancer wasn’t made for 10 months after seeing the first doctor and complaining about abdominal cramps, bloating, and pain. By the time she was diagnosed with ovarian cancer, it was stage IV.
right doctors and didn’t have the right tests performed. Her diagnosis of ovarian cancer wasn’t made for 10 months after seeing the first doctor and complaining about abdominal cramps, bloating, and pain. By the time she was diagnosed with ovarian cancer, it was stage IV.
Why is there no screening test?
No one has been able to identify a marker that would serve as an ovarian cancer screening test to find the cancer early or at a point before the cancer develops. In contrast, The Pap test and mammogram let us find pre-cancer or early cancer that can be treated effectively so the disease doesn’t advance and metastasize.
It is also difficult to palpate ovaries and masses (particularly in overweight women), and trans-vaginal ultrasound is not always specific and sensitive enough to detect ovarian cancer.
A protein called CA125, that’s found in greater concentration in ovarian cancer cells than in other cells of the body, can be measured from a blood sample. But the test has poor sensitivity and poor specificity for diagnosing ovarian cancer, so it’s primary value is to monitor patients with a known ovarian cancer. By checking the level of a patient’s CA125, the test can assess the effectiveness of chemotherapy.
CA125 is not a good screening test. About 50 percent of the cases with early stage ovarian cancer will have a normal CA125 and 25 percent who have advanced stage ovarian cancer will have a normal CA125. With those percentages, we might as well toss a coin!
Are MRIs at all effective in detecting ovarian cancer?
MRIs are very expensive and insurance companies won’t necessarily approve them, even if we have patients with known abnormalities.
Although advanced radiological means are letting us diagnose ovarian cancer earlier, MRIs and CT Scans are not typically employed as screening tests.
What factors put us at risk for ovarian cancer?

All doctors should take patients’ medical histories. Among women who have a higher degree of ovarian cancer are Ashkenazi Jews and those with a family history of breast or ovarian cancer, such as Angelina Jolie. Women who test positively for the BRCA1 or BRCA 2 mutations have up to a 40 percent lifetime risk of developing ovarian cancer.
Certain genetic mutations, other than those that are inherited, have also recently been linked to an increased risk for ovarian cancer. These findings could have important implications for developing better screening strategies for ovarian cancer and improving early detection.
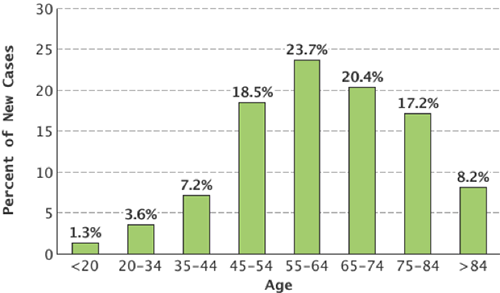
Age is another factor. Ovarian cancer rates are highest (23.7 percent) in women from 55 to 64 and the median age for detecting ovarian cancer is 63. Most masses are benign in younger women, but as a woman ages, there’s a higher likelihood that the mass will be cancerous. The ovaries of older women don’t experience the monthly changes they did when they were younger, so it’s less likely a mass will be the result of something other than cancer.
What should I expect to happen once an ovarian mass is detected and my doctor says it should be removed (whether or not it’s cancerous)?
Prior to removing a pelvic mass, an OBGYN must determine whether it’s likely to be benign or malignant. This can be done with a blood test called OVA1. The test was approved by the FDA is 2009 and detects the levels of various proteins, which increase or decrease in the presence of cancer.
The OVA1 test has a sensitivity of 96 percent (i.e. it is highly accurate in its ability to detect the disease even in its early stage), a negative predictive value of 95 percent (i.e. it is highly accurate in predicting the absence of disease).
The test can assess the likelihood that a mass is malignant before surgery. It can pick up things that a doctor can miss in his pre-operative impression. In clinical trials OVA1 identified 70 percent of malignancies missed by pre-surgical assessment alone.
It is important that a gynecologic oncologist operate on women with ovarian cancer. Over one million masses a year are seen in OBGYN practices and OVA1 helps us decide whether to refer a patient to a GYN Oncologist, who has additional training and experience in surgery on cancerous masses and whose treatment can result in better outcomes.

