I worry about getting
diabetes type 2.

My mother was diagnosed with it in her 70s, and her father had it, too, which I read increases my risk for contracting the disease. Most of us know that diabetes is a result of too much sugar in the blood, but did you know it can lead to complications including nerve damage in the feet, kidney and cardiovascular disease, skin issues and eye problems? When I felt slight tingling in my feet, on and off during the last few weeks, my concern escalated, since that’s listed among the symptoms. I’ve also been eating entirely too many sweets for a few months. Ice cream. Chocolate- covered graham crackers and pretzels. More ice cream.
 My last blood workup, at the end of 2016, didn’t show too much glucose (sugar) in my blood, but things like this can change in a matter of days, no less months, so I made an appointment with Dr. Donald A. Smith, an endocrinologist (a doctor who is involved with the various hormones and their actions and disorders in the body) and lipidologist (a doctor who is involved with lipids, the fats in your blood, and helps manage your cholesterol.) Diabetes is Dr. Smith’s specialty, and he went to Harvard Medical School, which I liked! I also liked that he’s been a doctor for decades. I’m not enamored with the younger crop of MDs, who want (and need) to get patients in and out of their offices in 15 minutes flat.
My last blood workup, at the end of 2016, didn’t show too much glucose (sugar) in my blood, but things like this can change in a matter of days, no less months, so I made an appointment with Dr. Donald A. Smith, an endocrinologist (a doctor who is involved with the various hormones and their actions and disorders in the body) and lipidologist (a doctor who is involved with lipids, the fats in your blood, and helps manage your cholesterol.) Diabetes is Dr. Smith’s specialty, and he went to Harvard Medical School, which I liked! I also liked that he’s been a doctor for decades. I’m not enamored with the younger crop of MDs, who want (and need) to get patients in and out of their offices in 15 minutes flat.
Besides having a new blood workup, I wanted to learn about diabetes, not just for myself, but for you, my FOFriends, because I read that adults over 45 years old are more at risk for it, “probably because people tend to exercise less, lose muscle mass and gain weight as they age,” reports the respected Mayo Clinic on its website. Over 28 million Americans have diabetes.
The facts about diabetes, according to the American Diabetes Association:
• Prevalence: In 2015, 30.3 million Americans, or 9.4% of the population, had diabetes; 23.1 million were diagnosed, and 7.2 million were undiagnosed
• Prevalence in Older People : About 25% of Americans age 60 or older (10 million) have diabetes (diagnosed and undiagnosed)
• New Cases: 1.5 million Americans are diagnosed with diabetes every year
• Prediabetes: In 2015, 84.1 million Americans age 18 and older had prediabetes
• Deaths: Diabetes remains the 7th leading cause of death in the United States in 2015, with 79,535 death certificates listing it as the underlying cause of death, and a total of 252,806 death certificates listing diabetes as an underlying or contributing cause of death.
These are grim statistics, so I was glad I was going to see Dr. Smith. I had to wait about an hour past my appointment time because he’s in great demand, but he spent over 75 minutes with me, getting my and my family’s medical history, studying the results of my last blood workup, examining me and giving me a crystal clear lesson about diabetes. Here’s what I learned:
 The cells in our body break down all sugars, such as sucrose (table sugar) and fructose (fruit sugar), to glucose. Glucose is a main source of energy for the cells that make up muscles and other tissues. It comes from food and from your liver, which makes and stores it.
The cells in our body break down all sugars, such as sucrose (table sugar) and fructose (fruit sugar), to glucose. Glucose is a main source of energy for the cells that make up muscles and other tissues. It comes from food and from your liver, which makes and stores it.
 Two blood values indicate whether diabetes is present in your body:
Two blood values indicate whether diabetes is present in your body:
A. Your Glucose Level: Normal glucose is under 100; anything between 101 and 125 means it’s slightly increased. It takes two values of 126 to be a definition of diabetes.
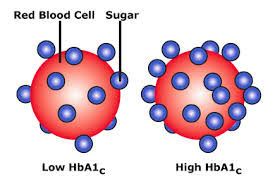
 B. Your Hemoglobin AIC Value: A1C measures the amount of hemoglobin (a protein inside our red blood cells that carries oxygen to the body) in our blood with glucose attached to it. Red blood cells love sugar (who can blame them), Dr. Smith explained.
B. Your Hemoglobin AIC Value: A1C measures the amount of hemoglobin (a protein inside our red blood cells that carries oxygen to the body) in our blood with glucose attached to it. Red blood cells love sugar (who can blame them), Dr. Smith explained.
Hemoglobin cells are constantly dying and regenerating, but they have a lifespan of two to three months, so the record of how much glucose is attached to your hemoglobin also lasts for about two to three months. If there’s too much glucose attached to the hemoglobin cells, you’ll have a high A1C. If the amount of glucose is normal, your A1C will be normal. The A1C test provides an average of your blood sugar readings for the past two to three months. It’s not accurate for any given day, but it gives the doctor a good idea of how effective your blood sugar control has been over time.
So what we know now is that normal A1C is 5.6% sugar or lower, and the definition of diabetes is 6.5% or higher, which means there is too much glucose in the blood, Dr. Smith told me. A level of 5.7 to 6.4% indicates prediabetes. “We want patients to be under 7%, because when your A1C goes from 8% to 7%, you have 40% fewer problems with eyes, nerves and kidneys. That’s why we try to control it carefully,” Dr. Smith explained. Glucose can rise to 180 in the two hours after you eat, but the A1C integrates these ups and downs. The American Diabetes Association provides a calculator that shows how A1C levels correlate to glucose levels.
 The beta cells that monitor the sugar in your body, helping to keep your blood sugar from getting too high (or low) are called insulin cells. If your sugar level rises, more insulin is put out. Insulin is a hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy, or to store glucose for future use.
The beta cells that monitor the sugar in your body, helping to keep your blood sugar from getting too high (or low) are called insulin cells. If your sugar level rises, more insulin is put out. Insulin is a hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy, or to store glucose for future use.

The pancreas secretes insulin into the bloodstream, then the insulin circulates to let sugar enter your cells. The insulin lowers the amount of sugar in the bloodstream. As your blood sugar level drops, so does the secretion of insulin from your pancreas. When your glucose levels are low, such as when you haven’t eaten in awhile, the liver produces glucose to keep your glucose level within a normal range.
This process doesn’t work well in type 2 diabetes, so sugar builds up in your bloodstream instead of moving into your cells. As blood sugar levels increase, the insulin-producing beta cells in the pancreas actually work harder to release more insulin, but eventually these cells become impaired and can’t make enough insulin to meet the body’s demands. You become insulin resistant. Your sugar levels rise.
Once insulin cells die out, you don’t get them back. “Then we have to do something, such as start you on medication, to increase the insulin. Or make what little insulin you have work better,” Dr. Smith added.
Note: Another blood test measures C-Peptide values, which shows your level of insulin-producing cells.
 You can help keep your insulin cells from dying out, and your A1C and glucose levels from rising, by following a low carbohydrate diet to lose weight, and start exercising, Dr. Smith advised. Carbs are fruits, grains, fast foods, vegetables, dairy and sweets, such as those on this chart. Each represents 15 grams of carbs.
You can help keep your insulin cells from dying out, and your A1C and glucose levels from rising, by following a low carbohydrate diet to lose weight, and start exercising, Dr. Smith advised. Carbs are fruits, grains, fast foods, vegetables, dairy and sweets, such as those on this chart. Each represents 15 grams of carbs.
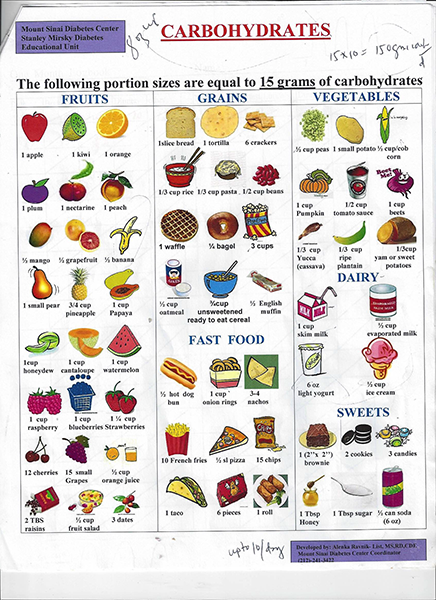
Dr. Smith explained that I can have up to 10 of the carbs shown on the chart, per day, or 150 carb grams a day. This is not like some of the wild diets where you eliminate carbs totally. “You want your weight to go down slowly,” Dr. Smith said. He also handed me a weekly weight recording chart and advised me to weigh myself, without clothes, only once a week, right after I get up and urinate.
 He also recommended a little book called The Calorie King, which gives you critical nutritional information on every food imaginable. Calorie King also offers a free app! “A little cookie might be 15 grams, but the book will tell you that an extra large cookie might be 75 grams,” Dr. Smith added.
He also recommended a little book called The Calorie King, which gives you critical nutritional information on every food imaginable. Calorie King also offers a free app! “A little cookie might be 15 grams, but the book will tell you that an extra large cookie might be 75 grams,” Dr. Smith added.
PS: My new blood results showed I don’t have diabetes, or even prediabetes. But, I do want to lose 15 pounds to insure I don’t get either. So, I started on the low carb diet the moment I left Dr. Smith’s office, exactly a week ago, and have lost 3 pounds! I can’t say I don’t miss the ice cream or chocolate-covered grahams, but that’s the price you pay for a healthier (and hopefully longer) life.

