This is a “sponsored post.” ellura compensated FOF with an advertising sponsorship to write it. Regardless, we only recommend products or services that we believe will be helpful for our readers. All insights and expressed opinions are our own.
Nan was endlessly miserable when she vacationed in Japan with her daughter Sophie in 2010. Urinary tract infections had been tormenting her for years, and the itching and burning returned full force on the trip. “I couldn’t enjoy even one peaceful hour,” Nan remembered. “I finally had to confess to Sophie what was going on.”
 Sophie is Dr. Sophie Fletcher, a urologist who deals with UTIs all the time, but her mom had never confided in her about her own. “She divulged that she’s been on and off antibiotics for years,” Sophie said. Although Sophie also would have prescribed antibiotic treatment back then, she was determined to find a different way to deal with Nan’s recurrent UTIs. Antibiotic resistance was a bigger and bigger medical problem every year, Sophie explained, and she wanted to take her mother off the drug merry go round.
Sophie is Dr. Sophie Fletcher, a urologist who deals with UTIs all the time, but her mom had never confided in her about her own. “She divulged that she’s been on and off antibiotics for years,” Sophie said. Although Sophie also would have prescribed antibiotic treatment back then, she was determined to find a different way to deal with Nan’s recurrent UTIs. Antibiotic resistance was a bigger and bigger medical problem every year, Sophie explained, and she wanted to take her mother off the drug merry go round.
“Antibiotics are wonderful, and we can’t survive without them, but they are not long-term options to reduce UTIs in women like my mother who suffer from recurrent infections,” Dr. Fletcher said. Rates of antibiotic resistance are rising dramatically all over the world, and the Centers for Disease Control recommends that physicians make it a top priority to reduce antibiotic use whenever possible, she added. “Judiciously prescribing antibiotics will prevent further resistance to them. Besides developing resistance, patients on daily antibiotics can develop long-term, irreversible side effects.”
EXTRACTING THE TRUTH ABOUT CRANBERRIES
Dr. Fletcher’s quest led her to a research team at Rutgers University that had discovered a chemical compound in cranberry extract which prevents UTI-causing bacteria from attaching to the bladder. “Women from generation to generation have been telling their daughters cranberry juice would protect them from urinary tract infections, assuming the acidity in the juice would kill the bacteria,” Dr. Fletcher said. Turns out an antioxidant phytonutrient –-proanthocyanidins (PAC)–does the trick. Researchers also determined the body requires 36 mg of PAC to consistently protect the urinary tract and bladder walls from bacteria leading to UTIs. “Even if you munched on dried cranberries and guzzled most brands of cranberry juice cocktail all day long, you still wouldn’t get the amount you need,” Dr. Fletcher emphasized.
 Fortunately, scientists developed a proprietary process to extract high levels of the potent
Fortunately, scientists developed a proprietary process to extract high levels of the potent
ingredient from the pure juice concentrate of cranberries. It’s available in a once daily, medical-grade supplement, called ellura that has 36 mg of PAC in every capsule, the minimum amount proven to prevent bacteria from adhering to the bladder and developing into a UTI. ellura currently offers a powerful punch – 36 mg PAC and maximum bacterial anti-adhesion activity.
Dr. Fletcher ordered ellura for her mom nine years ago, who hasn’t had a UTI since.
“Most supplements on the market contain less than 5 mg of PAC and most don’t include the PAC ingredient on their labels, just the milligrams of cranberry extract, which is irrelevant,” Dr. Fletcher said. The source of the 36 mg of PAC is also important; most supplements are made from the berry itself or from leftover seeds and stems, while ellura’s PAC is extracted from the pure juice concentrate to ensure its effectiveness. What’s more, many supplements are made with sugar and other ingredients that aren’t ideal for sensitive bladders or for diabetics. ellura has virtually no sugar.
ellura totally prevents UTIs in about 80 percent of Dr. Fletcher’s patients and significantly reduces UTIs in the remaining 20 percent. ellura is a proven solution and has the clinical data to confirm it. Left untreated, UTIs can move up to the kidneys and cause infection, and hospitalization, especially in the older population. Take Dr. Fletcher’s advice: “It’s really, really important to see your doctor if you have symptoms, take a urine test to confirm the diagnosis, and be treated with the appropriate antibiotic. Then the ellura is a must to prevent these UTIs from coming back.”
Let Nan’s experience with UTIs help you to take control of yours…. with ellura.
Enter code FAB at checkout for 25% off your first box or bottle (new customers only) through June.
DR. FLETCHER’S ABCs OF UTIs
➧ UTIs and Their Causes
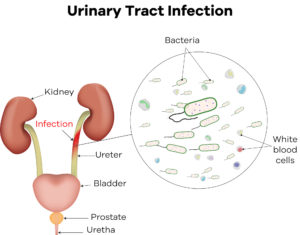 A UTI is an infection in any part of the urinary system, which includes the kidneys, ureters, bladder and urethra. Most infections involve the bladder and the urethra, which is the lower urinary tract. UTIs typically occur when “bad” bacteria, which normally live in the intestines, enter the urinary tract through the urethra, begin to multiply in the bladder, then take hold and grow into a full-blown infection. About 80 to 90 percent of UTIs are caused by E. coli bacteria. Approximately 50 percent to 60 percent of women will develop a UTI in their lifetimes.
A UTI is an infection in any part of the urinary system, which includes the kidneys, ureters, bladder and urethra. Most infections involve the bladder and the urethra, which is the lower urinary tract. UTIs typically occur when “bad” bacteria, which normally live in the intestines, enter the urinary tract through the urethra, begin to multiply in the bladder, then take hold and grow into a full-blown infection. About 80 to 90 percent of UTIs are caused by E. coli bacteria. Approximately 50 percent to 60 percent of women will develop a UTI in their lifetimes.
➧ The Symptoms of UTIs
 Symptoms come on very fast. First and foremost, you’ll feel distinct burning with urination, and pain, so you’ll know when you have it. You’ll also feel a constant pressure to urinate, but once you get to the restroom, little urine comes out. This is known as urinary frequency. Low back pain is the next most common symptom.
Symptoms come on very fast. First and foremost, you’ll feel distinct burning with urination, and pain, so you’ll know when you have it. You’ll also feel a constant pressure to urinate, but once you get to the restroom, little urine comes out. This is known as urinary frequency. Low back pain is the next most common symptom.
➧ The Different Types of UTIs
 Uncomplicated UTIs occur in patients with normal urinary tracts, both structurally and physiologically. Once a formal culture comes back positive from the laboratory, a doctor will treat this type of UTI with an antibiotic. Most women will get one or two uncomplicated UTIs in their lifetimes. It could come from just sitting on the beach for hours in a wet bathing suit, which creates a warm, moist environment that makes it easier for bacteria to enter the bladder.
Uncomplicated UTIs occur in patients with normal urinary tracts, both structurally and physiologically. Once a formal culture comes back positive from the laboratory, a doctor will treat this type of UTI with an antibiotic. Most women will get one or two uncomplicated UTIs in their lifetimes. It could come from just sitting on the beach for hours in a wet bathing suit, which creates a warm, moist environment that makes it easier for bacteria to enter the bladder.
 Uncomplicated recurrent UTIs are the same as uncomplicated UTIs, but occur three or more times during the year. This can be very disruptive, like it was for my mother on vacation. A physician usually gives a patient with recurrent UTIs a standing prescription for antibiotics so she can dash to the pharmacy when she feels the symptoms coming on. This is called self start therapy.
Uncomplicated recurrent UTIs are the same as uncomplicated UTIs, but occur three or more times during the year. This can be very disruptive, like it was for my mother on vacation. A physician usually gives a patient with recurrent UTIs a standing prescription for antibiotics so she can dash to the pharmacy when she feels the symptoms coming on. This is called self start therapy.
Woman with uncomplicated recurrent UTIs are sick and tired of repeated episodes of pain, trips to the doctor and taking time off from work. They’re always anxious about when their next UTI is going to strike, and they worry about what’s causing their infections. Patients frequently ask: ‘Why is this happening to me?’ We’ll always do a thorough work up with tests to make completely certain there’s nothing abnormal in a patient’s urinary tract. Unfortunately, many women are just prone to UTIs.
Uncomplicated recurrent UTIs only after sex are common, especially with sexually active women. Small amounts of the most common bacteria associated with UTIs already live in the vaginal area and can get pushed into the bladder with sexual intercourse. I recently saw a patient over 50 years old who gets a horrible UTI every time she has sex with her second husband. She’s at a point in her life where her immune system could be changing for some reason, and she isn’t able to fight off the bacteria entering her vagina like she did with her first husband when she was in her 20s and 30s.
I recommended ellura to this woman, and when she came back to see me she asked if I’d send ellura brochures to her primary care doctor so other woman with recurrent UTIs wouldn’t have to struggle like she did.
Uncomplicated recurrent UTIs in postmenopausal women might stem from a thinning of the tissue that lines the vagina and the outside of the bladder, declining cell turnover, and diminished glandular secretions as a woman ages and loses estrogen. These conditions can make the vagina less hospitable to “good “bacteria while creating a perfect breeding ground for the
“bad” E. coli bacteria which are more likely to invade the urinary tract and bladder.
Complicated recurrent UTIs are associated with either anatomic abnormalities of the bladder or the kidneys and will only end when the abnormality is corrected with surgery.
➧ Steps to Reduce The Risk of UTIs
Void normally and don’t hold your urine for long periods of time. Always use the restroom at normal three to four hour intervals.
 Stay well hydrated so you can urinate sufficiently. Some people are worried that if they drink too much water they won’t be able to get to a restroom in time, but hydrating properly helps to physically flush the bladder. Good electron microscopy studies have revealed that there are constant levels of some bacteria in the urine that move in and out of the female bladder. Those bacteria levels cannot grow once the next wave of urination comes along and you pee them all out.
Stay well hydrated so you can urinate sufficiently. Some people are worried that if they drink too much water they won’t be able to get to a restroom in time, but hydrating properly helps to physically flush the bladder. Good electron microscopy studies have revealed that there are constant levels of some bacteria in the urine that move in and out of the female bladder. Those bacteria levels cannot grow once the next wave of urination comes along and you pee them all out.
 Avoid sitting in a warm, moist environment for long periods of time, such as on the beach in a wet bathing suit and in a sauna.
Avoid sitting in a warm, moist environment for long periods of time, such as on the beach in a wet bathing suit and in a sauna.
Always wipe from front to back when you void, which moves the bacteria from the urethra back to the rectum, not the other way around. This is really important. You can’t wipe away all the bacteria because they’re microscopic, and you can’t sterilize yourself, but you can keep the stool, which contains e coli bacteria, towards the back as much as possible.
 Urinate right after sex if you’re prone to getting UTIs from intercourse. Thus will help flush the bacteria out of the bladder.
Urinate right after sex if you’re prone to getting UTIs from intercourse. Thus will help flush the bacteria out of the bladder.
Topical (vaginal) estrogen and probiotics for postmenopausal women can help thicken the vaginal lining, increase blood flow and normalize vaginal pH so the vagina is hospitable once again to “good” bacteria, which can help block the “bad” bacteria from adhering to it. Lactobacillus probiotics often are recommended to help prevent UTIs, but there’s no scientific evidence to support the best dosage, the best way to take them, or their efficacy.


